Fructose malabsorption is the current name for what used to be called ‘fructose intolerance’. The old name led to many people confusing the condition with another one called ‘hereditary fructose intolerance’
Hereditary fructose intolerance
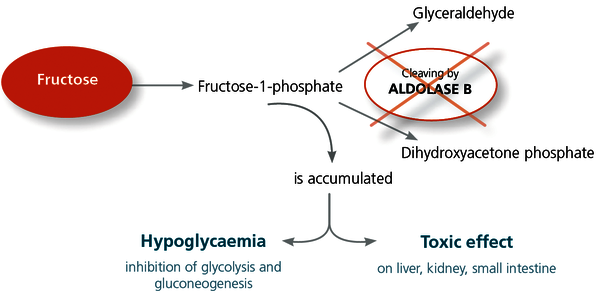
Hereditary fructose intolerance is a rare genetic condition, distinctly different from fructose malabsorption.
It affects around one in every twenty thousand people. It occurs because these people are lacking a specific enzyme required to break down fructose.
Hereditary fructose intolerance is very serious and often causes liver failure. Due to its nature, it is diagnosed during childhood, often when the baby is put on formula. The first indication is often failure to thrive.
Fructose malabsorption
Fructose malabsorption is much more common. It’s been suggested that up to one in three people are affected.
It occurs when the cells on the surface of the small intestine have difficulty breaking down fructose. Fructose-rich foods continue throughout the digestive system and are consumed by bacteria in the large intestine. That leads to fermentation, gas and a whole heap of symptoms.
- Abdominal distention
- A feeling of bloating
- Pain
- Reflux can occur due to upward pressure
- Irregular bowel motions – diarrhoea and constipation
Causes of Fructose Malabsorption
Fructose malabsorption is a fairly new condition, so the causes are not definitively confirmed. There is some evidence for a range of potential causes, including
- An imbalance of good and bad bacteria
- Inflammation within the digestive tract
- Stress, in all its different forms. So not just emotional stress, but any condition which causes stress on the body.
- Viral infections. Rotavirus, norovirus and adenovirus. There’s even some evidence that the Epstein Barr virus can trigger digestive issues.
- Gastro, either overseas or here in Australia.
- Excess intake of sugar and simple carbohydrates.
- Excess intake of processed foods, as preservatives can damage the microbiome.
- Chronic use of antibiotics, which is becoming more commonplace these days.
- Low stomach acid or the use of stomach acid suppressants
- Nutrient deficiency. Zinc, Vitamin A and protein are required for optimal health of the gut lining, so a lack of any of these in the diet may cause issues.
Diagnosing fructose malabsorption
Fructose malabsorption is diagnosed using a breath test. You can get a referral from your doctor or your naturopath.
Basically, they measure your hydrogen and methane levels in your breath. They take a baseline measurement, then you have a big cup of fructose – say 100 milligrams – and they measure your breath again. The test results depend on how the gas levels change.
Fructose Malabsorption and FODMAPs
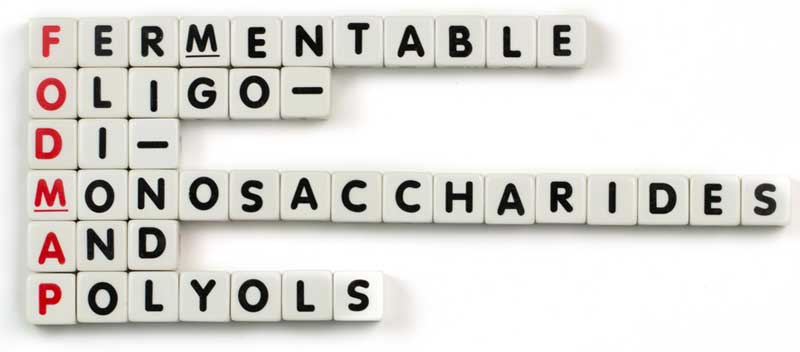
Many people diagnosed with fructose malabsorption are confused about whether they have to avoid just fructose or all FODMAPs.
FODMAPs stands for fermentable oligosaccharides, disaccharides, monosaccharides and polyols. These are basically different types of sugar and carbohydrate, which can be malabsorbed and cause symptoms.
The FODMAP diet was created to help manage fructose malabsorption.
If you’ve got a diagnosis of fructose malabsorption, you will need to cut your intake of all FODMAPs, at least initially. After a period of about four to six weeks, you can start slowly reintroducing FODMAPs, to determine what you can tolerate.